CT versus HRCT (High Resolution Computed Tomography), What Is The Difference?
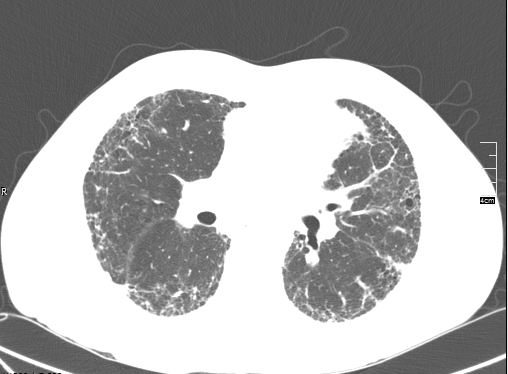
 HRCT (high resolution computed tomography) scans of the chest are crucial in the evaluation of idiopathic pulmonary fibrosis. A CT scan of the chest uses X-rays to obtain images of the lung tissue. The images are obtained in “slices” or thin views that are put together to form a picture. The slices of an HRCT are much thinner than with a standard CT scan giving a more detailed picture. One easy comparison is the difference between regular sliced bread and thinly sliced bread. Normal CT scans of the lungs create three to five millimeter slices of the lung tissue for evaluation. These slices are great for looking at the lung tissue for nodules or masses but not for appreciating the fine details. HRCT scans take one millimeter slices. The thinner slices allow for a much more detailed analysis.
HRCT (high resolution computed tomography) scans of the chest are crucial in the evaluation of idiopathic pulmonary fibrosis. A CT scan of the chest uses X-rays to obtain images of the lung tissue. The images are obtained in “slices” or thin views that are put together to form a picture. The slices of an HRCT are much thinner than with a standard CT scan giving a more detailed picture. One easy comparison is the difference between regular sliced bread and thinly sliced bread. Normal CT scans of the lungs create three to five millimeter slices of the lung tissue for evaluation. These slices are great for looking at the lung tissue for nodules or masses but not for appreciating the fine details. HRCT scans take one millimeter slices. The thinner slices allow for a much more detailed analysis.
How to Prepare for an HRCT Scan of the Chest
HRCT scans can be performed at outpatient imaging centers, as an outpatient appointment at a hospital, or as an inpatient at a hospital. There is usually minimal prep required and the imaging center or doctor’s office will give you specific instructions when scheduling the test. It is a good idea to wear comfortable clothing and leave all valuables such as jewelry at home the day of the test.
What to Expect During the HRCT
The patient will be placed on a flat table that moves in and out of a round donut-shaped machine. HRCT scans do not use contrast so there is no need for an IV. The patient will be positioned so that their chest is in the scanner. A CT scanner is open, the patient is not placed in a tube or enclosed space. The technicians performing the test will leave the room prior to the scan starting to avoid the radiation but will be able to monitor the patient through a glass window and intercom system. The patient will be asked to be as still as possible to create the best images. Instructions will be given on when the patient should breath and hold their breath during the scan. Patients being evaluated for idiopathic pulmonary fibrosis will be positioned prone and supine, meaning they will be positioned on their stomachs and on their backs. The scan usually takes between 15 and 30 minutes. There are no restrictions following the test. You will be able to return to normal activities, eat as usual, and drive yourself home.
What do the Results of an HRCT Show?
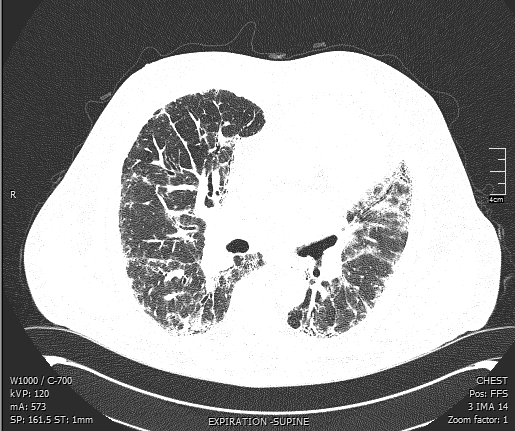
The results of the HRCT will be read by a radiologist. The images and the radiologist’s report will be sent to the ordering physician. Most physicians require their patients set a follow up appointment with them to review the results. During the follow up appointment your physician will be able to show you the “pictures” and discuss the specific findings. Characteristic findings of scarring or honeycomb changes at the bases of the lungs in the correct distribution (along the periphery of the lung) may be diagnostic of IPF and a lung biopsy might be avoided.
How Often Should HRCT Chest Scans be Done?
The frequency of HRCT scans for IPF patients is controversial. Twenty years ago, many pulmonologists would repeat these scans every six to twelve months. However, as we have come to appreciate the risks of radiation exposure there has been a trend away from frequent scanning. HRCT scans expose the patient to a lot more radiation than a standard chest X-ray. Many physicians choose to repeat the HRCT if they would change their plan of action based on the results. Looking for the sake of looking is not a great reason. Physicians can utilize other tests such as 6 minute walk tests or pulmonary function tests to measure disease progression.