Although we don’t have a clear understanding of why some people develop Idiopathic Pulmonary Fibrosis, a growing body of evidence has implicated Gastro-Esophageal Reflux (GER) as a an important co-factor in the development and progression of Idiopathic Pulmonary Fibrosis.
What is GER?
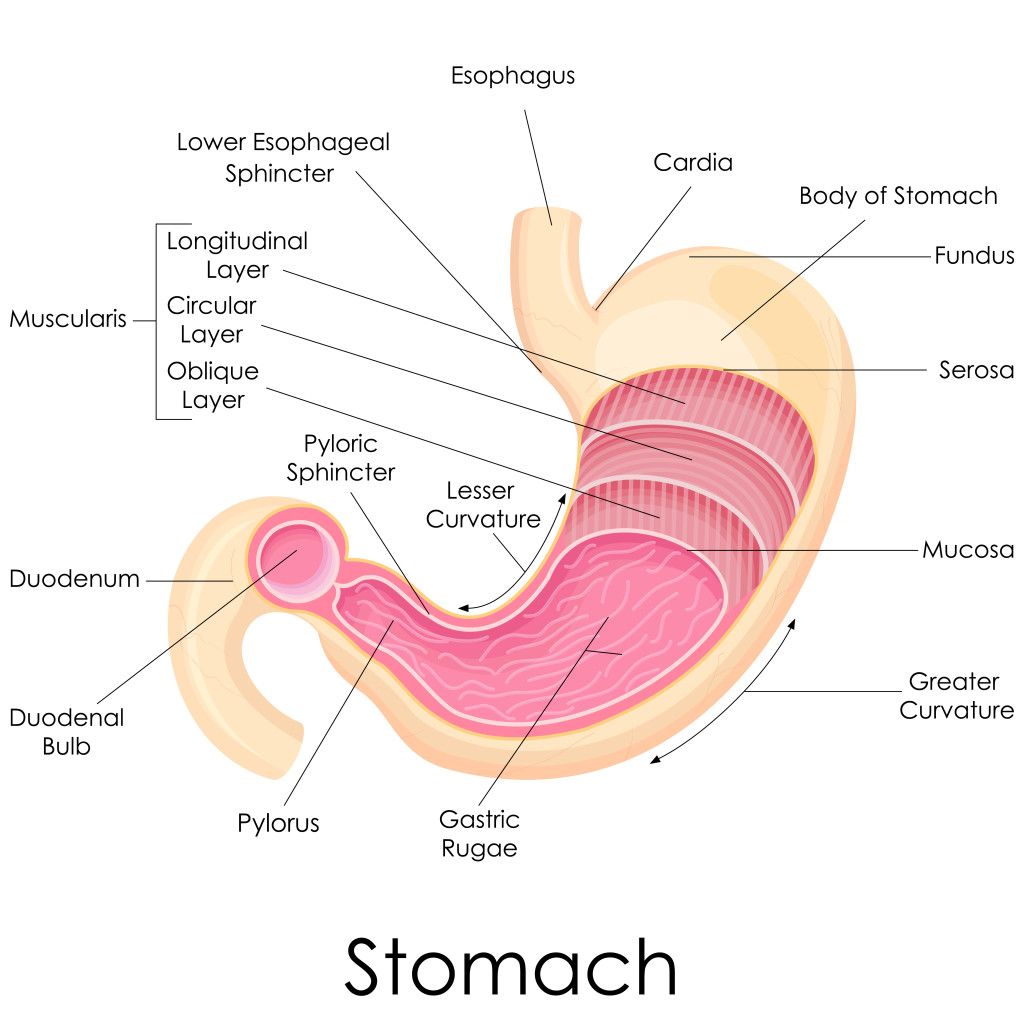 We normally put food into our mouth. Food is then passed into the esophagus by swallowing. The esophagus, which is a muscular tube, then conveys the food to the stomach where digestions begins. The stomach secretes acid and other chemicals to begin the digestion process. The stomach acts as a reservoir for holding food and releasing it at an appropriate rate into the small intestine. Separating the esophagus from the stomach is specialized muscular area or sphincter called the lower esophageal sphincter. This muscle transiently relaxes as food passes downward into the stomach and then contracts to prevent stomach contents from washing backwards into the esophagus.
We normally put food into our mouth. Food is then passed into the esophagus by swallowing. The esophagus, which is a muscular tube, then conveys the food to the stomach where digestions begins. The stomach secretes acid and other chemicals to begin the digestion process. The stomach acts as a reservoir for holding food and releasing it at an appropriate rate into the small intestine. Separating the esophagus from the stomach is specialized muscular area or sphincter called the lower esophageal sphincter. This muscle transiently relaxes as food passes downward into the stomach and then contracts to prevent stomach contents from washing backwards into the esophagus.
Gastro-esophageal reflux is the backwards movement of food and stomach acid into the esophagus. GERD or gastro-esophoageal reflux disease is also used to describe this process when heartburn is present. Most of the time, the esophagus has protective mechanisms such as coordinated contractions to limit any stomach contents from going beyond the lower portion of the esophagus but in patients with IPF, there is a high rate of stomach contents moving further upwards into the esophagus. In several studies, IPF patients had decreased function of the their lower esophageal sphincter. Furthermore, small amounts of the refluxed stomach contents may end up in the lungs, a process called micro-aspiration. This process of micro-aspiration is thought to be a disease driver in IPF. Unfortunately symptoms typical of heartburn such as chest discomfort or burning in the chest are not predictive of who is having GER. Said another way, many patients with IPF will be having silent, symptomless reflux of stomach contents into their lungs.
What can be done about GER in IPF?
There are several interventions that can dramatically improve GER. An analysis of IPF patients that had their GER treated showed slower decline in lung function, less fibrosis on CT scans and improved survival compared to patients that were untreated.
1. Acid suppressing medications
Acid suppressing medications such as H2 blockers and Proton Pump inhibitors decrease the acidity of the stomach. This makes any fluid that does end up in the lungs less irritating to the lungs. H2 blockers that I recommend include famotidine (Pepcid) and ranitidine (Zantac). Both are taken twice daily and are equally effective. There are very few side effects with H2 blockers and they can be obtained over the counter without a prescription. I do not recommend cimetidine (Tagamet) due to drug interactions and side effects.
Proton pump inhibitors include (PPIs) omeprazole (Prilosec), esomeprazole (Nexium), pantoprazole (Protonix), rabeprazole (Aciphex), and lansoprazole (Prevacid). These medications are taken either once or twice daily. Side effects can be seen with PPIs and include loss of magnesium and an increased risk of osteoporosis and bone fractures. Supplemental magnesium is often administered to minimize this risk. Other side effects include an increased risk of gastro-intestinal infections. Many PPIs can be obtained over the counter without a prescription. You should check with your doctor to make sure that there are no interactions with your other medications. This is especially true for patients taking Clopidogrel (Plavix).
PPIs are more powerful than H2 blockers. I typically place IPF patients on once daily PPI and recommend magnesium oxide 400mg once daily. In patients that are taking Clopidogrel, I would start with an H2 blocker twice daily.
2. Diet changes
Avoid caffeine, alcohol, citrus, spicy, and fatty foods. All of these foods relax the lower esophageal sphincter and promote GER.
3. Avoid late night meals and snacks.
Having a full stomach before you lie down promotes GER. Allow 3 hours after you eat before you recline fully or lie down. Make dinner a smaller meal and lunch a bigger meal.
4. Elevate the head of your bed at least 10 inches.
This can be achieved with a foam wedge under your mattress or wood blocks under the feet of your bed at the head of the bed. An adjustable mattress also works well. Propping yourself up on pillows is not very effective. During the night, most patients periodically slide off the pillows.
Surgery for GER
There are several surgical procedures that can be performed to limit GER. The most common is called a Nissen Fundoplication. This surgery involves wrapping the top part of the stomach around the inlet to the stomach to create a tighter lower esophageal sphincter. This procedure is quite effective in the short term but studies comparing this procedure to long-term medications don’t show consistent advantages. Patients with advanced pulmonary fibrosis are not good surgical candidates.
In the evaluation for lung transplantation, much attention is paid to the presence of GER. A body of data suggests that GER after lung transplantation increases the likelihood of chronic rejection. Nissen fundoplication may be performed after transplantation if needed, provided the esophagus is working normally.