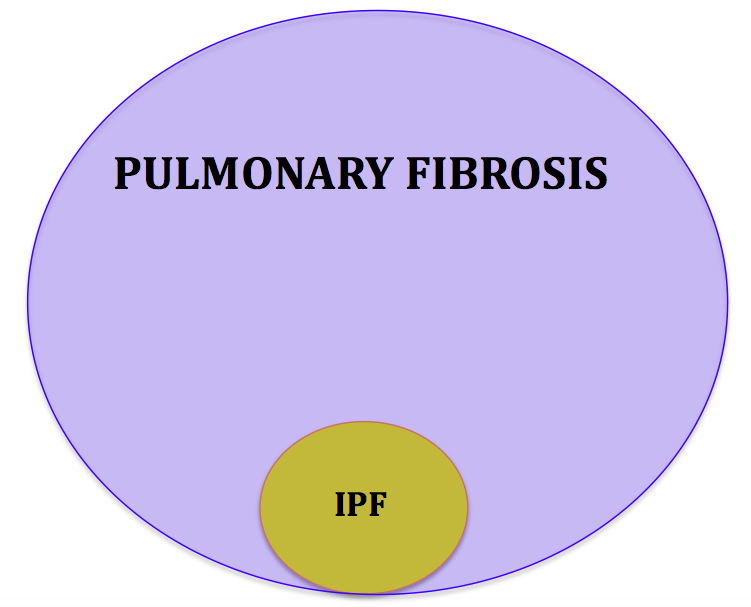
We have received a variety of questions about pulmonary fibrosis that is not Idiopathic Pulmonary Fibrosis (IPF). The terminology is quite confusing in this area of medicine. IPF is a very specific diagnosis that is only a small portion of the universe of pulmonary fibrosis. Most patients with pulmonary fibrosis have non-IPF pulmonary fibrosis.
Many types of lung injuries can lead to scarring in the lungs. When seen on CT scans, these areas of scarring are referred to as pulmonary fibrosis by some radiologists. For example, although most episodes of pneumonia resolve without any permanent injury to the lungs, in some cases, small areas of scarring can remain. This type of pulmonary fibrosis is not progressive and has an excellent prognosis. We recognize this pattern by the patchy distribution and lack of other abnormal lung findings. Serial imaging if performed will show that these areas of scarring do not change over time. Pulmonary function testing is usually only mildly abnormal and does not worsen with time. I often worry about recurrent gastro-esophageal reflux (GER) and recurrent aspiration of stomach contents into the lungs.
Patients that have had radiation therapy for cancer that included some lung tissue in the treatment field can have areas of scarring in the lungs. This is also a non-progressive form of lung scarring.
There is a large family of lung disorders that are broadly referred to as interstitial lung disease. This family includes many diseases such as non-specific interstitial pneumonitis, lymphocytic interstitial pneumonitis, desquamative interstitial pneumonitis, pulmonary langerhans cell hystiocytosis, sarcoidosis, hypersensitivity pneumonitis and others. Each disease has a characteristic pathology under the microscope and findings on high resolution CT scanning that are suggestive and at times diagnostic. As these diseases progress, they causes scarring or fibrosis in the lungs. Each of these lung diseases has a different course, treatment strategy and prognosis.