A pulmonary embolism, or PE, involves a blood clot that breaks loose from another area of the body and travels to the lungs. Some research indicates that having pulmonary fibrosis increases a person’s risk of developing a pulmonary embolism as a result of venous thromboembolism (VTE).
What is a Pulmonary Embolism?
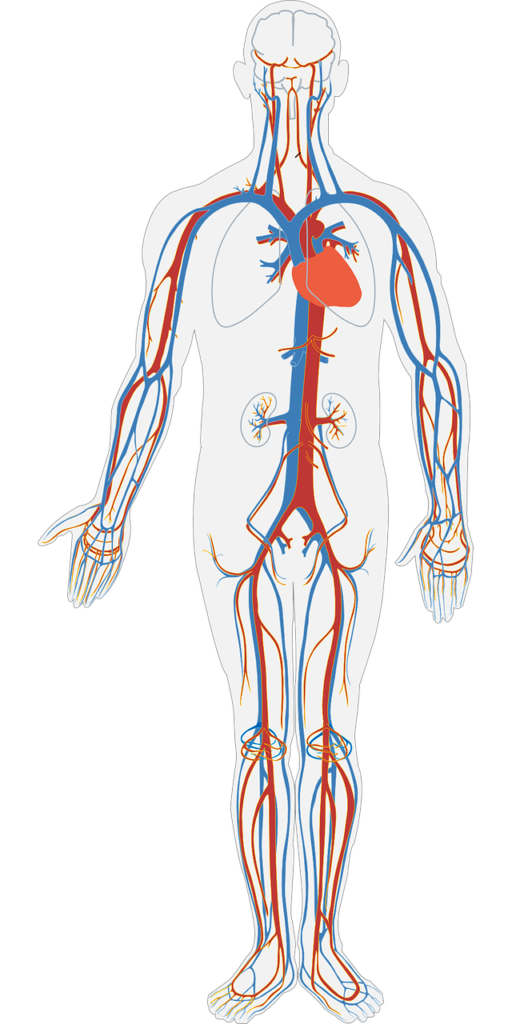
A VTE is a blood clot that develops in a vein. In many cases, a blood clot develops in the lower legs. Part of the clot may break off and travel into the pulmonary artery in the lungs, which prevents the blood supply to the lungs. When this occurs, the condition is referred to as a pulmonary embolism.
In one large study, which involved over 200,000 people with idiopathic pulmonary fibrosis, 3815 people with IPF also had a diagnosis of VTE. The results indicated that the risk of developing a VTE was 34 percent higher in people with IPF than in the general population.
Although a connection between developing a PE and IPF has not been definitively established, it appears there is probably an increased risk of VTE and pulmonary embolisms in people with pulmonary fibrosis.
The specific physiological reason people with IPF may develop blood clots more often than the general population is not fully understood. But regardless of the cause, if you have IPF and develop a pulmonary embolism, it can be a life-threatening situation.
A pulmonary embolism is serious for everyone. But in people with IPF, they have less lung capacity, which means even a small blood clot in the lungs can lead to serious problems.
In some cases, if you have other risk factors for a blood clot such as surgery or a hip or leg fracture, your doctor may prescribe blood thinners to decrease your risk of developing blood clots. If you have a history of developing a VTE or PE, your doctor may also suggest blood thinners as a preventative measure for future clots. If you develop a blood clot, it may be treated with blood thinners and medications called thrombolytics to dissolve the clots.
Symptoms of a Venous Thromboembolism
It’s important to recognize the symptoms of a blood clot so it can be treated as soon as possible to prevent complications. Symptoms of a clot may include:
- Swelling in the leg
- Pain in the calf or thigh
- Skin that is warm to the touch
- Red streaks on the skin
Symptoms of a Pulmonary Embolism
If a clot travels to the lungs and causes a PE, it’s essential to seek immediate medical treatment. Symptoms of a PE can include:
- Increased respiratory rate
- Rapid heart rate
- Chest pain (which may be worse when breathing in)
- Lightheadedness
- Shortness of breath (more than normal for you)
- Decreased oxygen level
Prevention of VTE and PE
There are a few things you can do to reduce your risk of developing blood clots including the following:
If possible, avoid prolonged immobility: Avoid sitting for long periods of time. For example, when traveling, get up and walk or stretch your legs and do ankle circles when possible.
Don’t smoke: Smoking is thought to increase a person’s risk of developing a blood clot. Plus, smoking also leads to additional airway damage, which is extremely detrimental for people with IPF.
Maintain a healthy weight: According to the American Heart Association, people that are obese have twice the risk of developing a blood clot than those that are a healthy weight.
Content written by Dr. Jeremy Feldman, an expert in Idiopathic Pulmonary Fibrosis, with contributions by MaryAnn DePietro, B.S. CRT, a licensed respiratory therapist.