We appreciate our readers submitting questions. We try and choose a selection to answer that is representative of common issues in IPF.
GERD and IPF
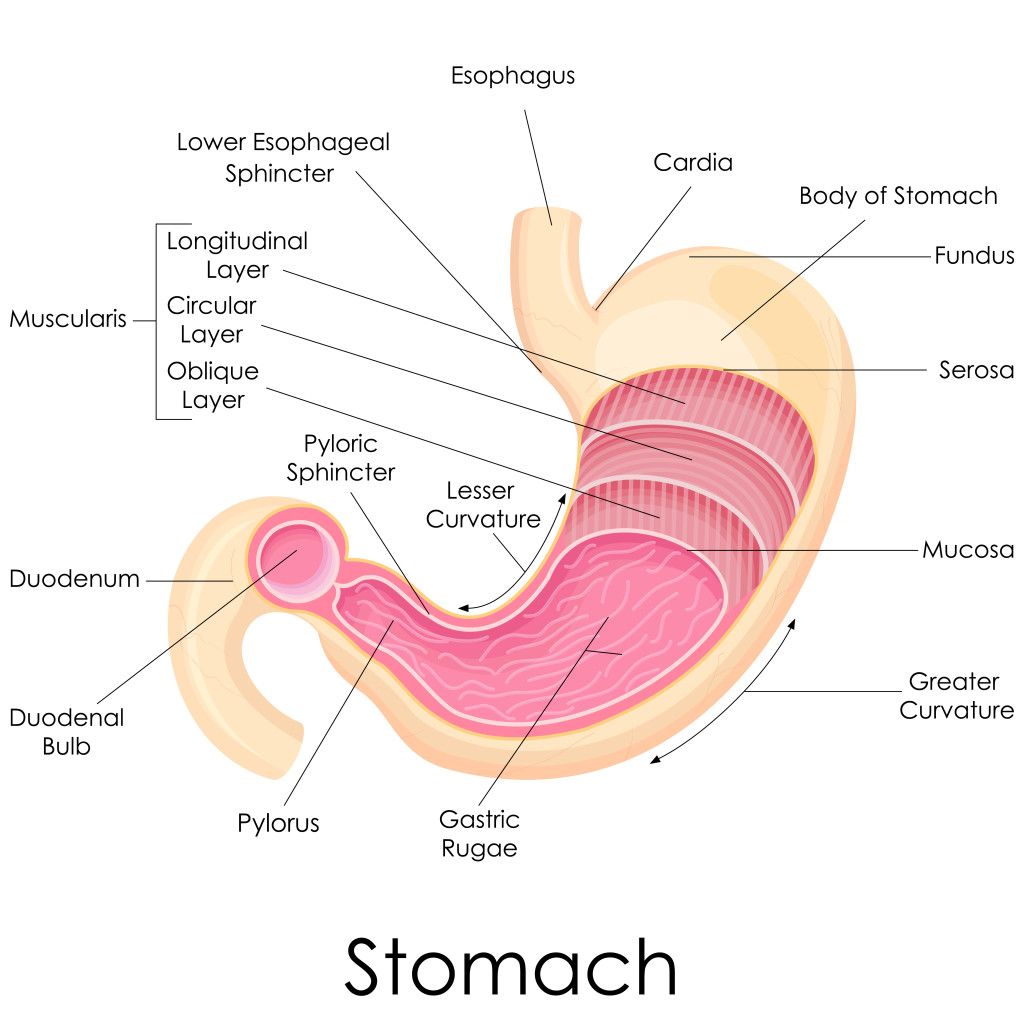
We receive many questions about GERD (gastro-esophageal reflux disease) and IPF. This has been a very controversial area of research in IPF. There is good quality data that GERD symptoms and signs of GERD on invasive testing are much more common in patients with IPF than age-matched healthy adults.
What remains unclear is whether the reflux causes IPF and we have not been able to show convincingly that treating GERD consistently improves the course of IPF. My general approach is to look for GERD in patients with IPF. I believe that we have become too focused on pills to treat problems rather than changing behavior. In GERD, diet often plays a huge role. Removing caffeine, citrus, alcohol, spicy foods, deep fried foods, late meals, large meals often is much more important that taking a pill to reduce stomach acid production. Elevating the head of the bed also may be very helpful. In patients who continue to have problems adding acid suppressing medicines is reasonable. For more details about GERD and IPF click here.
Fatigue and IPF
We have written extensively about cough and IPF and shortness of breath. We have not written much about fatigue in patients with IPF. Fatigue can be a disabling symptom in patients with lung disease. Patients often ask what causes the fatigue. The short answer is that there are many contributing causes:
- Low oxygen levels with activity
- Increased work of breathing results
- Decreased blood flow through your heart from pulmonary hypertension
- Poor sleep quality
- Emotional stress (anxiety/depression/worrying)
- Deconditioning (your muscles get out of shape)
Strategies to reduce fatigue involve addressing the above issues. Use your oxygen when you are active. Ask your doctor to consider if you might have pulmonary hypertension. Work on improving your sleep quality (your pulmonologist or primary care doctor will have suggestions). Take time to tackle the emotional hurdles of having IPF. Don’t neglect your muscles. Many patients benefit from pulmonary rehabilitation (structured exercise programs supervised by respiratory therapists).
Environment and IPF
We often receive questions about whether certain environmental exposures can make IPF worse. As we don’t have a precise understanding of the causes of IPF it is difficult to give a precise answer. However, my general advice is as follows:
- Avoid high altitude. The higher you go the less oxygen in the air. This leads to lower blood oxygen levels for everyone but especially for patients with IPF. If you have a pulse oximeter you can measure your oxygen levels. Using supplemental oxygen can help but you will still feel more short of breath and have reduced exercise capacity.
- Avoid poor air quality. Patients with IPF (or any chronic lung disease) already have lungs that are not working properly. Avoid dusty environments, smoke exposure and pay attention to air quality warnings from the health department.
- Avoid extremes of temperature. My patients consistently tell me that hot/humid conditions and very cold conditions make them feel worse.