How is Idiopathic Pulmonary Fibrosis Diagnosed?
The diagnosis of Idiopathic Pulmonary Fibrosis requires a careful patient health history, physical exam and a battery of tests. Every patient being screened for idiopathic pulmonary fibrosis should have a chest X-ray, a high resolution CT (HRCT) scan of the chest, full pulmonary function tests (PFTS), a six-minute walk test and some blood work. Some physicians request that patients being screened for IPF have an arterial blood gas (sampling of blood from the radial artery) and some patients will need a lung biopsy.
Important Criteria Used to Diagnose IPF
 The patient should be in the correct age group. This disease is almost never diagnosed in patients less than 40 years old and the majority of patients are over 50 years old.
The patient should be in the correct age group. This disease is almost never diagnosed in patients less than 40 years old and the majority of patients are over 50 years old.
- A detailed history of exposure to asbestos and other chemicals is also very important. Asbestos can lead to pulmonary fibrosis (scarring of the lungs) that is very similar to IPF.
- Patients in general should have either cough or shortness of breath.
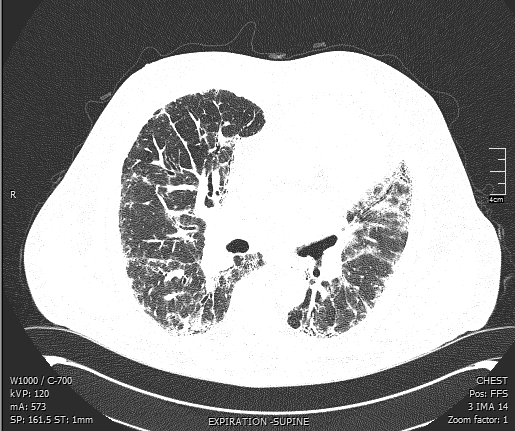
- Imaging tests of the lung such as HRCT (high resolution computed tomography) scans may be diagnostic if all the right characteristics are present. However, for many patients, the diagnosis requires a lung biopsy. This is done with a minimally invasive surgery called a VATS (video assisted thoracoscopic surgery). A lung biopsy with an expert lung pathologist evaluating the specimens under a microscope is currently the gold standard for diagnosis.
Traditionally the diagnosis of IPF required a lung biopsy done by a surgeon under general anesthesia. In the past 20 years, we have learned that many patients can be confidently diagnosed based on a special type of CT scan of their chest. If this HRCT (high resolution computed tomography chest) shows the characteristic findings of scarring or honeycomb change at the bases in the correct distribution (along the periphery of the lung) then a biopsy is not needed. Unfortunately, many patients do not have the required findings on their scans and a lung biopsy is required.
Blood Tests Cannot Diagnose IPF
 Unfortunately at this time there is not a specific blood test that can confirm the diagnosis of idiopathic pulmonary fibrosis. Physicians may order blood tests to look for signs of infections that might be contributing to a patients shortness of breath or they may order an arterial blood gas to see how much oxygen a patient is carrying in their blood.
Unfortunately at this time there is not a specific blood test that can confirm the diagnosis of idiopathic pulmonary fibrosis. Physicians may order blood tests to look for signs of infections that might be contributing to a patients shortness of breath or they may order an arterial blood gas to see how much oxygen a patient is carrying in their blood.
Bronchoscopy : Not The Test of Choice for Idiopathic Pulmonary Firbrosis
Often physicians order a bronchoscopy when their patients present with complaints of cough or shortness of breath. Bronchoscopy involves using a flexible thin camera to inspect the airways and to obtain very tiny pieces of lung tissue. This is performed under light sedation (twilight or conscious sedation). The camera is advanced either through the nose or mouth through the vocal cords into the airways. Washings for culture may be obtained. Biopsy of the lung tissue can be performed (transbrochial biopsy). This involves placing a tiny flexible forceps through the bronchoscopy into the airway and pinching a tiny piece of lung tissue. The size of the biopsy is about ¼ of a small grain of rice. Due to the very small size of the biopsies, this technique is not acceptable or useful in making the diagnosis of IPF. Other diseases such as sarcoid and hypersensitivity pneumonitis may be diagnosed in this way but not IPF. If your lung doctor is most worried about IPF then transbrochial biopsy of the lung is not the best approach.
When is bronchoscopy helpful?
- When infection is a concern
- When Sarcoid or HP is a concern. Both of these can be diagnosed about 75% of the time by bronchoscopic lung biopsy
When is bronchoscopy not helpful?
- When IPF is the most likely diagnosis
- Distinguishing IPF from nonspecific interstitial pneumonitis
- Just to “take a look”
 Surgical Lung Biopsy Can Definitively Diagnose IPF
Surgical Lung Biopsy Can Definitively Diagnose IPF
In contrast to a transbrochial biopsy, a surgical lung biopsy (often called VATS for video assisted thoracoscopic surgery) is done under general anesthesia. A surgeon inserts two small telescope-like ports into the chest. Through these ports, small instruments can then be used to obtain much larger pieces of tissue. Ideally 3 pieces from 2 lobes of the lung should be submitted. The tip of the middle lobe is generally avoided.